Explore our lineup.
Black
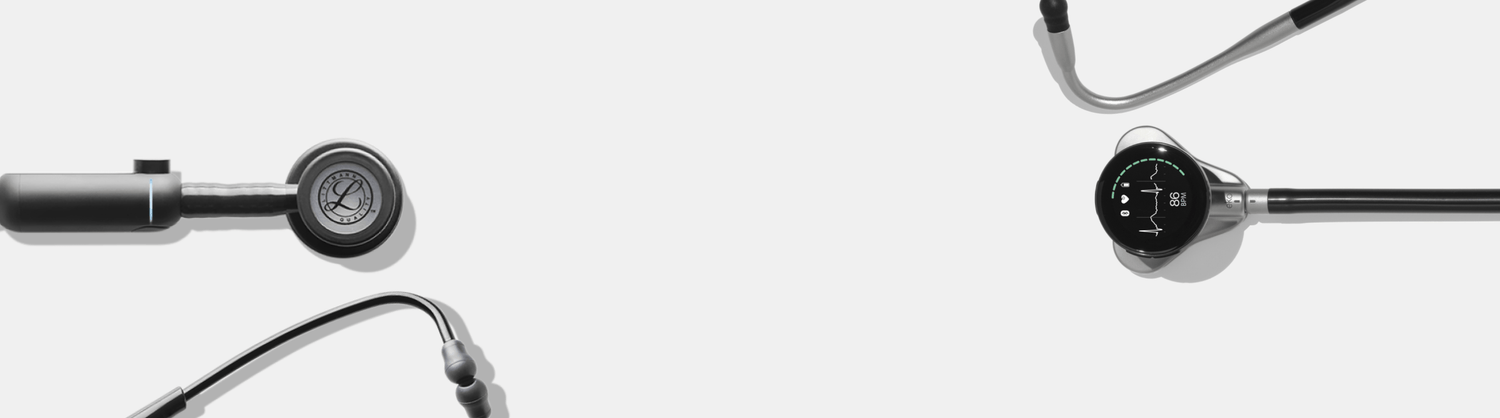
Eko CORE™ Digital Attachment
Attachment that transforms your analog stethoscope to digital with amplification and noise cancellation.
$259
$209
SHOP NOW
Black
High Polish Rainbow
High Polish Copper
High Polish Mirror
3M™ Littmann® CORE Digital Stethoscope
Littmann® cardiology-grade stethoscope enhanced by Eko's CORE™ digital technology.
$379
$349
SHOP NOW
Silver
Matte Black
Champagne
Amethyst
Wintergreen
Sapphire - Black
Electric Pink
Eko CORE 500™ Digital Stethoscope
The modern stethoscope replacement, blending 3-lead ECG with AI insights like AFib and murmur detection.
$449
$389
SHOP NOW
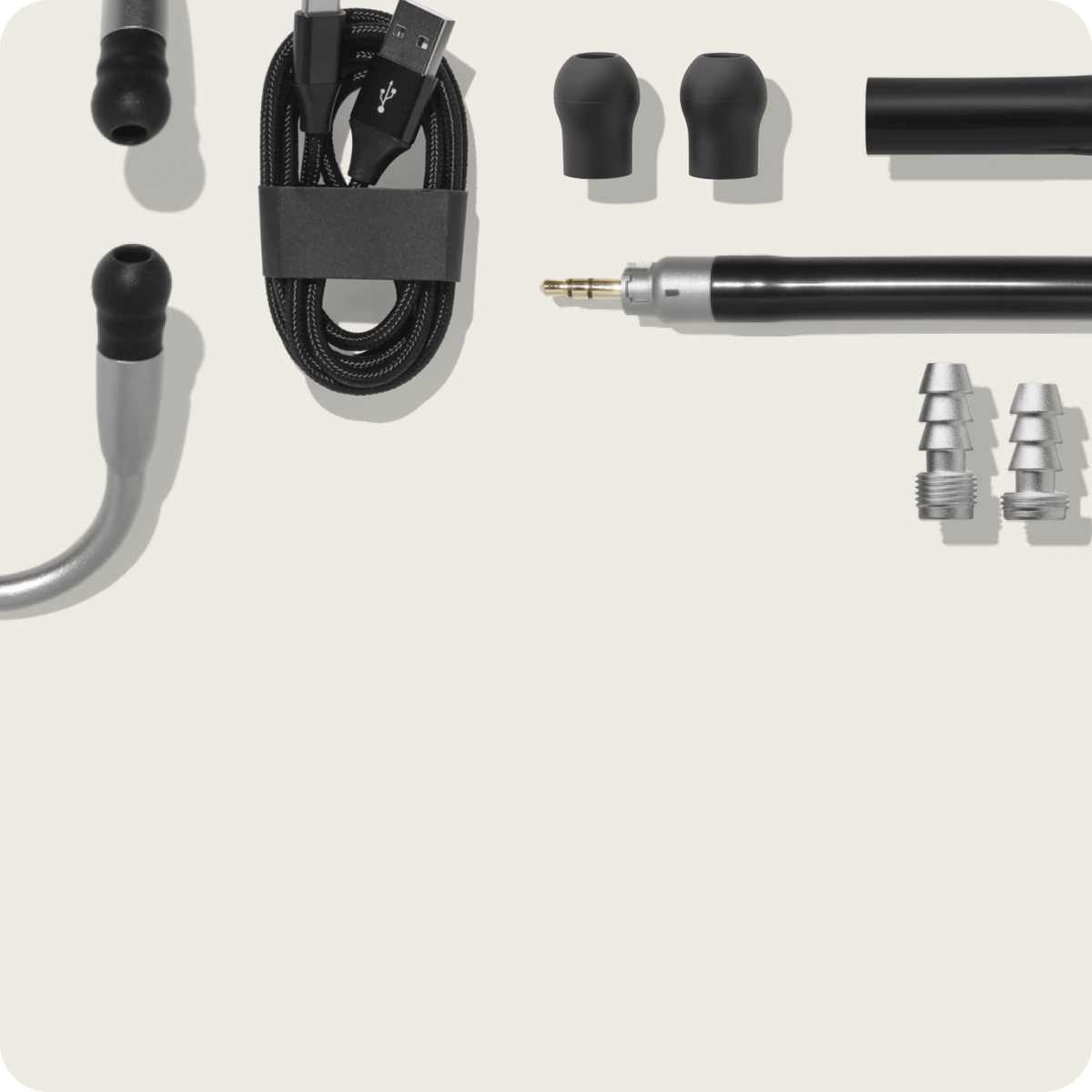
Accessorize your stethoscope.
MKT-0003672